Abstract
Introduction: Despite good initial responses, many multiple myeloma (MM) patients eventually relapse post autologous hematopoietic cell transplant (AHCT). Risk stratification to Identify patients that are at an increased risk of early relapse may influence post-AHCT monitoring and selection of maintenance therapy. Recently, the Center for International Blood and Marrow Transplant Research (CIBMTR) scoring system was introduced as a tool to identify patients at risk of early relapse post-AHCT. The scoring system relies on each patient's albumin level at time of MM diagnosis, bone marrow plasma cell (BMPC) percentage at time of AHCT, and cytogenetic risk profile to classify them into three risk categories. Here, we aimed to test the validity of the CIBMTR scoring system by applying it to our cohort.
Methods: We reviewed all patients who underwent AHCT for MM at Cleveland Clinic between 2011-2021, and then identified the patients with available data to be incorporated into the CIBMTR system. As per the scoring system's requirements, points were assigned for the following patient characteristics: 4 points for high risk (HR) cytogenetics, 4 points for BMPC ≥10% at AHCT, 2 points for albumin <3.5 g/dL at diagnosis, 1 point for standard risk (SR) cytogenetics, 0 points for normal cytogenetics, BMPC <10% at AHCT, and albumin ≥3.5 g/dL at diagnosis. Baseline demographic, clinical, and cytogenetic data of the included patients were retrospectively collected by reviewing electronic medical records to compare the three risk groups. Analysis was conducted through multivariate analysis using the Statistical Package for Social Sciences (SPSS), while median overall survival (mOS) and median progression free survival (mPFS) of the three groups were analyzed using GraphPad Prism.
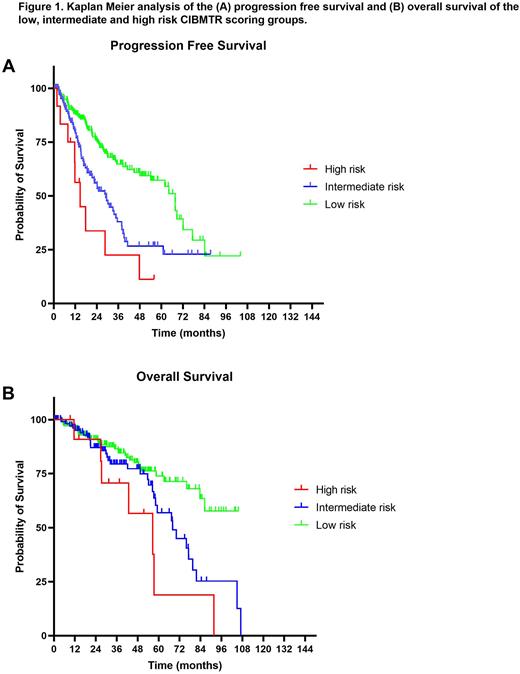
Results: A total of 313 patients met inclusion criteria and were included in our study. Our cohort had a median age of 61.7 years at AHCT, a 57.2% male preponderance and a median follow up of 31.9 months. With regards to the CIBMTR scoring system constituents, 106 (33.9%) had HR cytogenetics as compared to 146 (46.6%) with SR and 61 (19.5%) with normal cytogenetics. Albumin ≥3.5 g/dL occurred in 85 (27.2%) while BMPC ≥10% were present in 31 (9.9%). CIMBTR risk score application yielded 191 (61%) patients classified as low risk (score 0-3), 110 (35.2%) patients as intermediate risk (score 4-8), and 12 (3.8%) patients as high risk (score 9-10) of early relapse after AHCT. There were no significant differences between the low-, intermediate and high-risk groups with respect to median age at transplant (61 vs 63.1 vs 62.3%, P=0.1), Gender representation (Males 56.5 vs 60 vs 50%, P=0.7), Ethnicity (White 82.2 vs 86.4 vs 91.7%, P=0.5), median lines of therapy pre-AHCT (P=0.3), or remission status (partial/very good partial/complete) pre-AHCT (P=0.17). Compared to low- and intermediate-risk patients, respectively, patients belonging to the high-risk group had higher 1-year relapse (41.7 vs 10.5 vs 18.2%, P=0.0043), 2-year relapse (58.3 vs 17.8 vs 38.2%, P=0.0001) and 3-year relapse (66.7 vs 25.7 vs 50.9%, P<0.0001) rates. Kaplan-Meier based survival analysis confirmed a lower mPFS in the high-risk group compared to the low- and intermediate-risk groups, respectively (14.7 vs 67.7 vs 29 months, P<0.0001) (Fig 1A). Interestingly, the CIBMTR score also distinguished the three risk groups with respect to overall survival. High-risk patients had higher mortality at the 5-year (50 vs 15.7 vs 22.7%, P=0.0082) and 7-year (58.3 vs 17.3 vs 29%, P=0.0008) follow up intervals as compared to low- and intermediate-risk patients, respectively. Kaplan-Meier analysis further corroborated the mortality rates since high-risk patients had lower mOS relative to intermediate- and low-risk patients, respectively (56.6 vs 68 vs unreached, P=0.0046) (Fig 1B).
Conclusion: We validated the CIBTMR scoring system criteria within an internal cohort, demonstrating that this system is a reliable tool for identification of patients with a higher risk of early relapse post-AHCT. We further identified differences between risk groups in mortality at 5- and 7-years following AHCT.
Disclosures
Kurish:Market Access Transformation: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal